Clinical Documentation
The Clinical Documentation tools in VEHRDICT are designed to help providers capture patient encounters clearly, efficiently, and in compliance with clinical standards. Whether you're documenting a routine visit or a complex medical history, VEHRDICT provides a range of features to support thorough and accurate charting. This guide explains how to use the different parts of the documentation system.
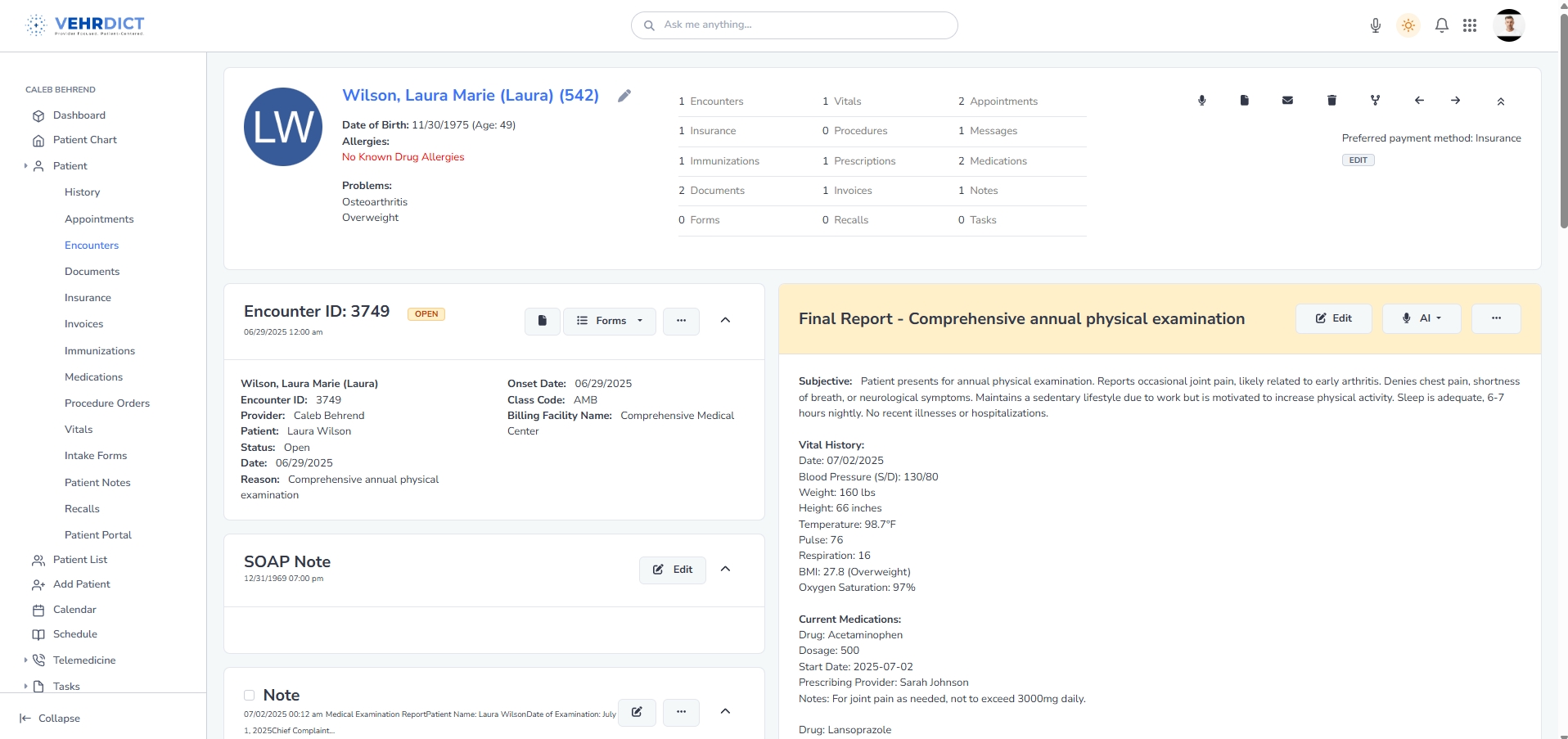
SOAP/encounter notes
SOAP notes in VEHRDICT follow the standard format of Subjective, Objective, Assessment, and Plan. When starting a new encounter, you’ll be able to enter information into each section using free-text, templates, or voice input. Notes can be saved as drafts and updated later if needed. Once finalized, the encounter note is stored in the patient’s chart and can be viewed or printed at any time. This format keeps documentation structured and easy to follow for both providers and auditors.
Progress notes
Progress notes are used to document updates between full encounters or track changes in a patient’s condition over time. These notes are often shorter than SOAP notes and can be added as standalone entries in the patient’s record. VEHRDICT allows you to tag progress notes by date, provider, and category, which makes them easy to search and organize. These notes help ensure continuity of care and support follow-up planning.
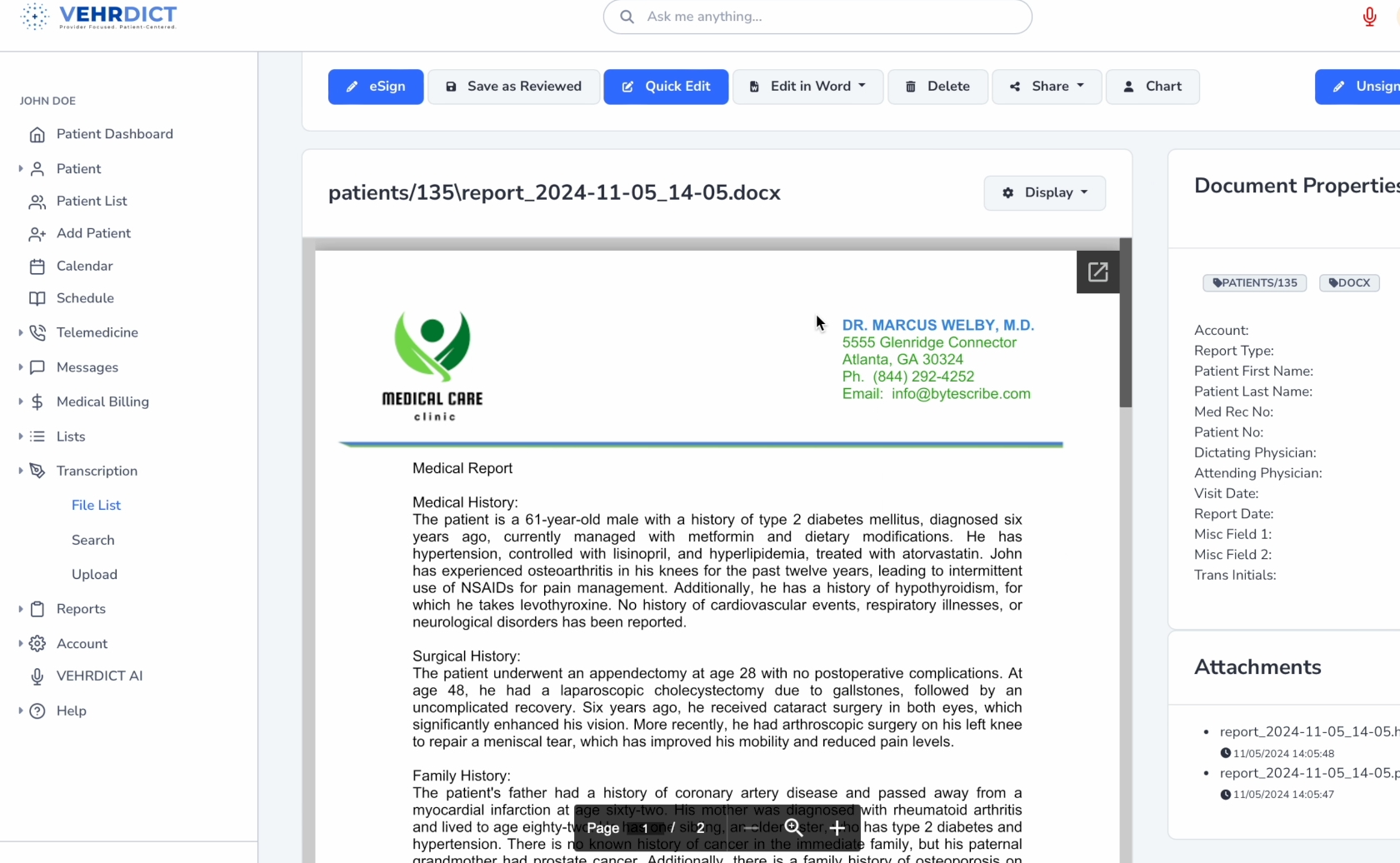
Medical history
The medical history section contains information about past diagnoses, surgeries, medications, allergies, and family history. You can enter this information manually or import it from previous encounters or scanned documents. VEHRDICT keeps this information in a centralized location within the patient chart so it's always accessible during new visits. Keeping an accurate and up-to-date history is essential for safe treatment and clinical decision-making.
Templates and forms
VEHRDICT includes a variety of templates for different specialties, procedures, and visit types. You can select a template when starting a new encounter or create custom templates to suit your workflow. These templates populate fields with standard phrasing or prompts, making documentation faster and more consistent. You can also attach forms—such as functional assessments or screening tools—to an encounter and complete them digitally during the visit.
AI-assisted documentation
To speed up and simplify charting, VEHRDICT offers AI-assisted documentation. As you enter notes or dictate information, the AI can automatically structure the content, suggest relevant details to include, and format the final document into a clean, professional layout. It can also flag missing sections that are typically required for coding or compliance, helping reduce omissions. This feature is especially useful for maintaining consistency across providers and improving overall documentation quality.
Clinical decision support
VEHRDICT includes clinical decision support tools that provide helpful prompts and alerts during documentation. These can include drug interaction warnings, reminders for preventive care, or guidance based on documented diagnoses. The system cross-references patient data in real time to suggest evidence-based actions or highlight potential issues. These tools are built into the documentation workflow to help support safer, more informed care without disrupting the provider's process.
Clinical documentation in VEHRDICT is designed to streamline and enhance the way healthcare providers capture patient information during encounters. The system offers a structured yet flexible interface that supports both voice-driven AI input and traditional manual form entry. This ensures that clinicians can document efficiently in their preferred workflow without compromising accuracy or compliance. VEHRDICT supports the entire documentation process, from initial data capture to final report generation, making it a central hub for clinical records.
One of the core strengths of VEHRDICT lies in how it effortlessly aggregates data from multiple sources to build a comprehensive and accurate clinical narrative. During an encounter, information may come from patient intake forms, past medical history, real-time dictation, or even recorded interviews. VEHRDICT intelligently compiles all this data, minimizing manual entry and reducing the risk of omissions or inconsistencies. This consolidated data forms the basis of the final patient document, ensuring that all relevant details are available in one place.
The EHR’s AI capabilities further elevate the documentation process by automatically organizing the collected information into a polished, professional report. VEHRDICT formats each document according to medical standards and best practices, ensuring it is ready for patient communication, internal use, or audits. Beyond formatting, the AI acts as a clinical guide—prompting the physician to include necessary elements required for regulatory compliance, insurance audits, and quality reporting. This helps maintain high documentation standards while reducing the administrative burden on clinicians.