X12 Partners
X12 Partner List
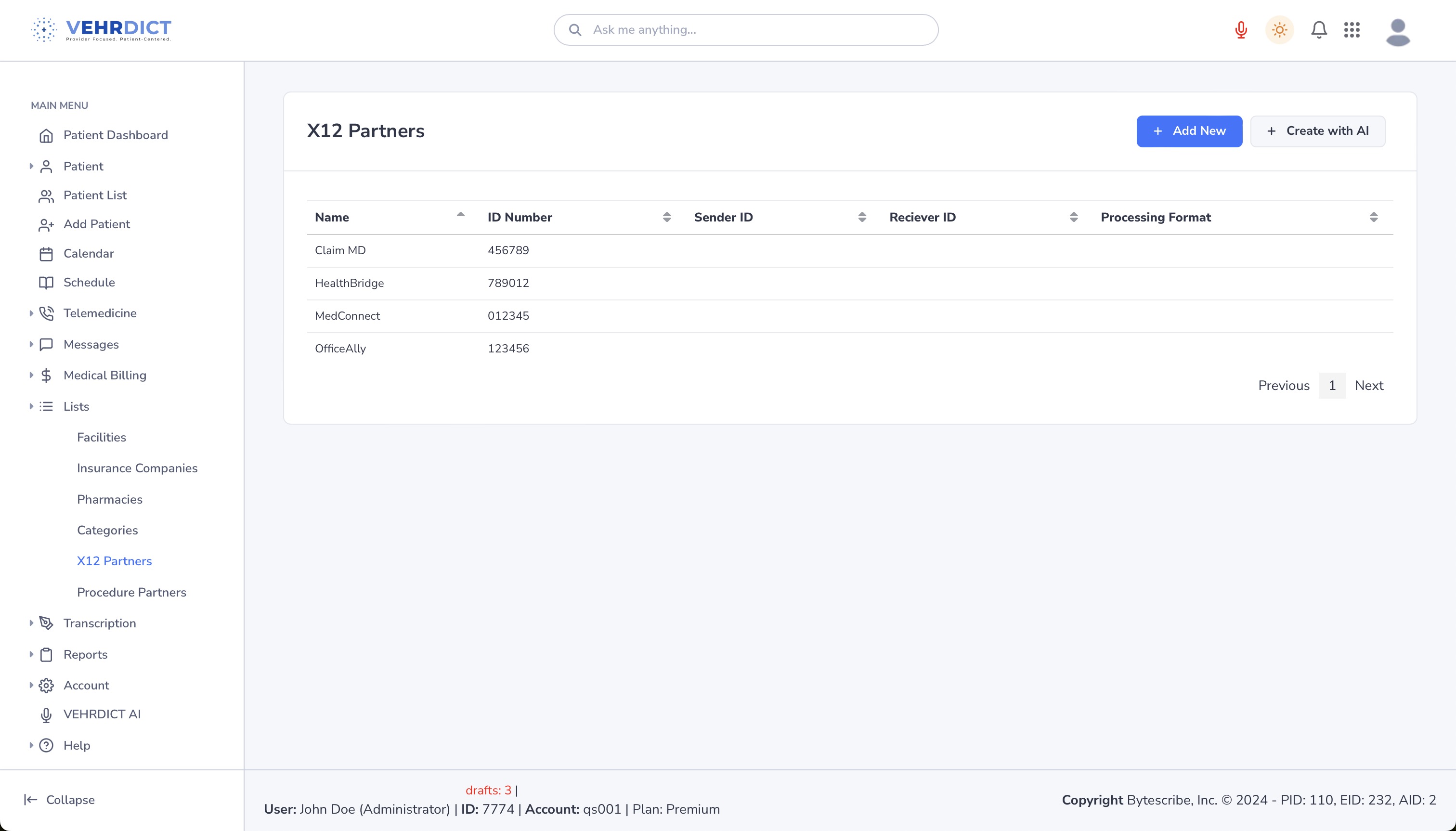
The X12 Partner List in the VEHRDICT system serves as a centralized hub for managing all electronic healthcare transactions with external entities, including insurance companies, clearinghouses, and government payers. This configuration is essential for enabling Electronic Data Interchange (EDI), which supports critical workflows such as billing, eligibility checks, remittance posting, and authorization requests.
Why X12 Partners Matter
The X12 Partner List plays a foundational role in ensuring:
- Accurate and timely claims submission (837)
- Seamless remittance processing and payment matching (835)
- Instant eligibility verification and coverage checks (270/271)
- Efficient authorization requests (278)
- Secure and trackable electronic exchanges between your system and payers
>
Tip: Verify payer ID accuracy for each X12 partner to avoid claim denials and transmission errors.
Accessing the X12 Partner List
To configure or review existing partners:
- Go to Lists → X12 Partners
- You'll be presented with a table listing existing partners, including:
* Partner Name * Payer ID * Connection Type * Transaction Types Supported (837, 835, etc.) * Status (Active/Inactive)
Adding a New X12 Partner
To add a new trading partner:
- Click the Add New button in the top right corner.
- Fill in the required fields:
* Partner Name
* Payer ID (from your clearinghouse or payer directory)
* EDI Endpoint (URL or connection ID for secure transmission)
* Supported Transactions – Select which X12 formats are supported:
* 837 (Claims Submission)
* 835 (Remittance Advice)
* 270/271 (Eligibility Requests & Responses)
* 278 (Prior Authorization Requests)
- Optional fields include:
* Notes/Contact Info for payer representative * File Formats – ANSI, X12N, or custom configurations * Custom Mappings – Specify if certain fields need to be remapped or filtered per partner
Editing or Deactivating a Partner
To update a partner:
- Select the X12 partner from the list
- Edit any field such as contact info, supported transactions, or payer ID
- Click Save to apply changes
If the partner is no longer in use, toggle the Active status to Inactive. This keeps the record for future reference without cluttering active options during claims submission.
Benefits of Proper X12 Configuration
- Faster claims submission and response times
- Fewer denials due to incorrect payer IDs or transmission errors
- Consolidated view of all payer relationships
- Improved revenue cycle transparency and control
- Direct integration with VEHRDICT’s Billing, Claims, and Insurance modules
>
Tip: For best performance, review your X12 Partner List regularly and deactivate obsolete or duplicate records.